大於一歲的小兒
氣管內管 Size 選擇 : (Age/4) + 4
氣管內管 Size 選擇 : (Age/4) + 4
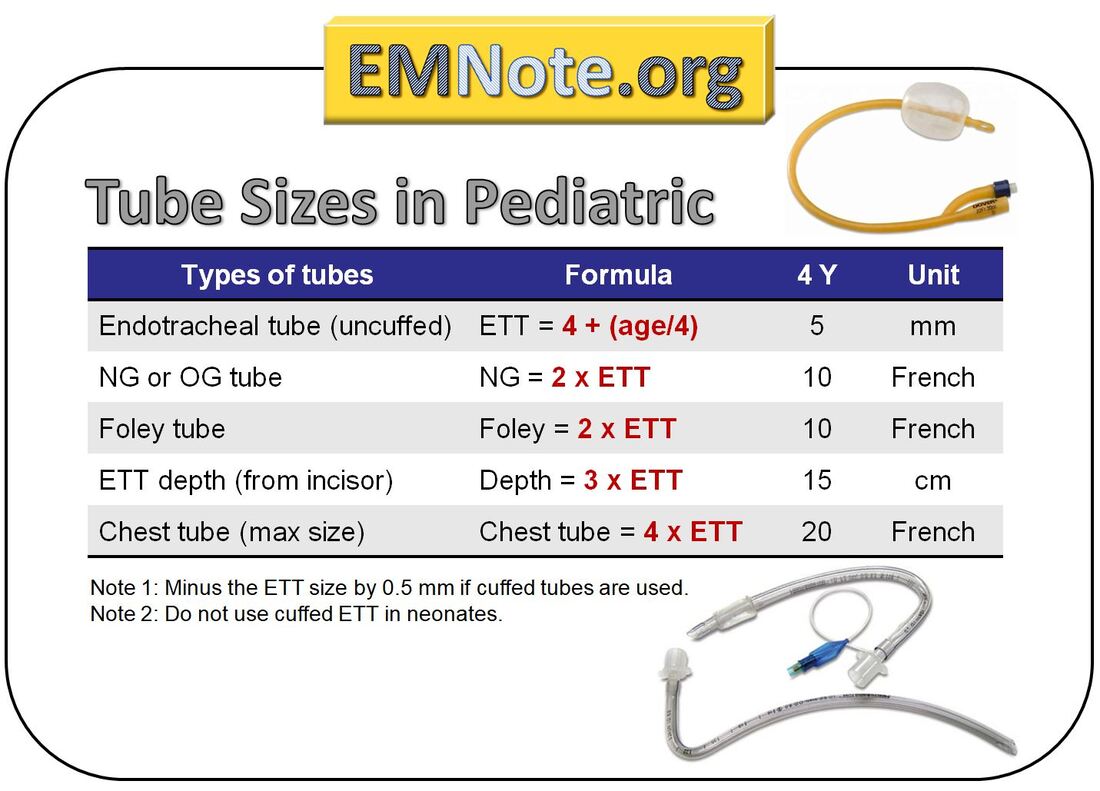
- 2 x ETT = NG or OG or Foley
- 3 x ETT = Depth of ETT
- 4 x ETT = Chest tube (max size)
https://www.emnote.org/


Positioning infants and children for airway management :
1. Align the glabella horizontally with the chin.
眉間 - 下巴
眉間 - 下巴
2. Open the anterior neck space.
3. Align the external auditory meatus
horizontally with the suprasternal notch.
外耳道 - 胸骨
horizontally with the suprasternal notch.
外耳道 - 胸骨
Chaper 113
Intubation and Ventilation of Infants and Children

Alignment of the oral, pharyngeal, and tracheal axes,
to allow visualization of the glottis,
is affected by several features most pronounced in the infant :
is affected by several features most pronounced in the infant :
(1) A relatively large head and occiput,
(2) A disproportionately large tongue and small mandible, and
(3) A larynx that is more cephalad and thus appears more anterior than in adults.
This acute angle can be overcome by extending the infant's neck
(unless cervical injury is suspected)
(unless cervical injury is suspected)
and, in some cases, placing a small roll under the shoulders. 墊脖子
The narrowest point of the child’s trachea is at the cricoid ring.
Surgical cricothyrotomy is contraindicated in children < 10 years old
because the cricothyroid membrane is too small.
because the cricothyroid membrane is too small.
Therefore, in children<10 years of age,
needle cricothyrotomy is the subglottic, invasive airway of choice.
needle cricothyrotomy is the subglottic, invasive airway of choice.
Common errors in pediatric BMV include
excessive ventilatory rate, inspiratory pressure, and volume.
excessive ventilatory rate, inspiratory pressure, and volume.
Thus, providers should generally squeeze the bag
only enough to allow for chest rise
only enough to allow for chest rise
in order to prevent gastric insufflation and barotrauma.
In infants and younger children,
a supine position usually causes flexion of the neck due to the large occiput,
a supine position usually causes flexion of the neck due to the large occiput,
and elevation of the shoulders or thorax is helpful to align the airway.
For children,the addition of a nasal cannula to other
preoxygenation techniques may also be beneficial,
although the flow needs to be relatively high
at 10 - 15 L/min for larger children
and 5 L/min for children under 1 year of age.
and 5 L/min for children under 1 year of age.
Fluid bolus (20 mL/kg normal saline)
is often beneficial before initiation of rapid-sequence intubation.
is often beneficial before initiation of rapid-sequence intubation.
Push-dose vasopressors : Epinephrine
drawing 1 mL of 1:10,000 epinephrine
and adding 9 mL of normal saline
and adding 9 mL of normal saline
to produce a 1:100,000 solution (10 micrograms/mL);
administer 0.1 mL/kg (1 microgram/kg) bolus doses
s needed to maintain blood pressure > 70 × (2 + age).
s needed to maintain blood pressure > 70 × (2 + age).
Although in practice, pediatric emergency medicine and critical care
have largely adopted rocuronium as the paralytic of choice.
have largely adopted rocuronium as the paralytic of choice.
Succinylcholine can cause fatal hyperkalemia in a number of conditions
In children, there is no evidence to support the use of pretreatment agents.
Bradycardia in children is typically a sign of hypoxia,
which should be corrected.
Atropine does not prevent succinylcholine-associated bradycardia
and should not be given prophylactically.
Difficult pediatric airways :
Acute upper airway infections,
such as epiglottitis and retropharyngeal abscesses;
acute airway obstructions, such as foreign bodies, trauma, or burns;
congenital anatomic airway abnormalities, such as Pierre Robin syndrome;
and airways contaminated with significant amounts of body fluids.
Consider supraglottic airway devices when ventilation with BMV
is inadequate and attempts at endotracheal intubation fail.
Cricothyrotomy :
Open surgical cricothyrotomy is not an option
in children < 10 years old due to the small cricothyroid membrane.
Needle cricothyrotomy is therefore recommended in children < 10 years old.
14-gauge needle + Ventilation through the catheter
using a 3.0-mm endotracheal tube adapter
jet ventilation may not be the ideal technique for trans tracheal ventilation
and should never be used in children <5 years old.
文章標籤
全站熱搜


 留言列表
留言列表


